A 40 yr old male with shortness of breath
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Name: G Sai Manogna
Hall ticket No: 1701006046
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION:
A 40 years old male, painter by occupation, resident of bhongir has presented to the casualty with the chief complaints of
- Shortness of breath since 7 days
- Chest pain on left side since 5 days
Personal historyDiet- MixedAppetite- Decreased since 7 daysBowel and bladder movements- RegularSleep- AdequateAddictions-Patient is a chronic smoker since 20 years- 5 cigarettes/day, but stopped 3 years agoAlcohol - Consuming whisky since 20 years- 90 ml each time, but stopped 3 years agoNo history of drug or food allergies
Family historyNo similar complaints in the family
General examinationDone after obtaining consent, in the presence of attendant with adequate exposurePatient is conscious, coherent, cooperative and well oriented to time, place and personPatient is well nourished and moderately built
No history of pallor, cyanosis, clubbing and lymphadenopathy
VitalsTemperature- AfebrileBlood pressure- 120/80 mm of HgPulse rate- 78 bpmRespiratory rate- 45 cpmSpO2- 91% at room air
Local examination:Respiratory system examination:
InspectionShape of chest is ellipticalB/L asymmetrical chestTrachea is in central positionExpansion of chest- Right normal; Left decreasedUse of accessory muscles seen (Neck muscles are used)
PalpationAll inspectory findings are confirmedNo local rise of temperature Trachea is deviated to right
Measurements:AP- 24 cmsTransverse- 28 cmsRight hemithorax- 42 cmsLeft hemithorax- 40 cmsCircumferental- 82 cms
Tactile vocal fremitus- Decreased on left side ISA, InfraSA, AA, IAA
PercussionDull note present in left side ISA, InfraSA, AA, IAA
AuscultationB/L air entry present, vesicular breath sounds are heardDecreased intensity of breath sounds in left SSA, IAAAbsent breath sounds in left ISA
Cardiovascular system examination:S1, S2 sounds are heardNo murmursJVP normalApex beat normal
Perabdominal system examination:Soft, non tenderNo organomegalyBowel sounds heardNo guarding, rigidity
Central nervous system examination:No focal neurological deficitsGait- normalReflexes- normal
Provisional diagnosis:Left sided pleural effusion with diabetes mellitus since 3 years
Investigations:FBS- 213 mg/dlHbA1C- 7%
Hb- 13.3mg/dlTC- 5600 cells/cummPLT- 3.57
Serum electrolytesNa- 135 mEq/LK-4.4 mEq/LCl- 97 mEq/L
Serum creatinineSerum creatinine- 0.8 mg/dl
LFTTB- 2.44 mg/dLDB- 0.74 mg/dLAST- 24 IU/LALT- 09 IU/LALP- 167 IU/LTP- 7.5 gm/dLALB- 3.29 gm/dL
Serum LDHSerum LDH- 318 IU/L
Blood ureaBlood urea- 21 mg/dL
Pleural fluidProtein-5.3 mg/dLGlucose-96 mg/dLLDH- 740IU/LTC- 2200DC- 90% lymphocytes10% neutrophils
According to lights criteria (To know if the fluid is transudative or exudative)
NORMAL:Serum Protein ratio: >0.5Serum LDH ratio: >0.6LDH>2/3 upper limit of normal serum LDHProteins >30gm/L
My Patient:Serum protein ratio:0.7Serum LDH: 2.3
INTERPRETATION: As 2 values are greater than the normal we consider as an EXUDATIVE EFFUSION.
(confirmation after pleural fluid c/s analysis)
Chest X-ray
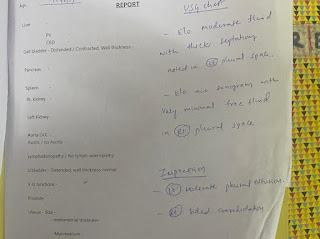
USG
ECG
2D EchoMedication- O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
- Inj. Augmentin 1.2gm/iv/TID
- Inj. Pan 40mg/iv/OD
- Tab. Pcm 650mg/iv/OD
- Syp. Ascoril-2tsp/TID
- DM medication taken regularly
Advice- High Protein diet
- 2 egg whites/day
- Monitor vitals
- GRBS every 6th hourly
(confirmation after pleural fluid c/s analysis)
- O2 inhalation with nasal prongs with 2-4 lt/min to maintain SPO2 >94%
- Inj. Augmentin 1.2gm/iv/TID
- Inj. Pan 40mg/iv/OD
- Tab. Pcm 650mg/iv/OD
- Syp. Ascoril-2tsp/TID
- DM medication taken regularly
- High Protein diet
- 2 egg whites/day
- Monitor vitals
- GRBS every 6th hourly







Comments
Post a Comment