G. Sai Manogna
Roll No 33
This is an online E logbook to discuss our patient's de-identified health data shared after taking her guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from an available global online community of experts to solve those patient's clinical problems with collective current best evidence-based inputs. This e-log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box are welcome.
Following is the view of my case: A 45-year-old woman, a farmer by occupation from Nalgonda has come to the OPD with the chief complaints of
* Fever for 3 days
*Vomitings since 2 day
*ALtered sensorium since 1 day
History of presenting illness:
In the month of February 2021, the patient has experienced lower abdominal pain for which she visited a hospital and was diagnosed as CA cervix and then hysterectomy was done after which the patient was normal.
She was apparently asymptomatic 3 days ago and then developed a high-grade fever which was insidious in onset and intermittent in type and was associated with chills and rigours
H/o vomiting 2 days ago with 5-6 episodes per day which was non-bilious, non-projectile, non-blood-tinged and were semi solid in consistency
Patient has come to the OPD with loss of alertness,disorientation, poor judgement or thinking and disturbances in perception and behaviour
The patient was taken to an outside hospital where she was diagnosed as NS1 dengue positive and was referred to Kamineni for further management
Past history:
There were no similar complaints in the past
Not a known case of Diabetes, Hypertension, Asthma, Tuberculosis, Epilepsy
Surgical history- Hysterectomy was done 6 months ago
No known allergic history
Personal history:
Diet- Vegetarian
Appetite- Decreased
Sleep- Adequate
Bowel and bladder movements - Regular
Addictions- None
Family history:
No significant family history
General examination:
Patient was not conscious, incoherent and non cooperative and is not oriented to time, place, and person Well nourished and moderately built
The GCS score is as follows:
Eye opening is spontaneous
No verbal response
Motor response- Normal flexion
Pallor- Absent
Icterus- Absent
Cyanosis- Absent
Clubbing- Absent
Lymphadenopathy- Absent
Edema- Absent
Vitals:
Temperature: Afebrile
PR- 62 bpm
BP- 110/80 mmHg
RR- 22 cpm
SPO2- 98%
Systemic examination:
Cardiovascular system:
*S1, S2 sounds were heard
*No abnormal murmers
Respiratory system:
*Position of trachea is central
*Bilateral air entry positive
Per abdomen:
*The abdomen is soft, non distended and non tender
*No organomegaly
*No palpable mass or fluid present
Central Nervous Examination:
Patient is unconscious
1. Higher mental functions
*Level of consciousness - Unconscious
*Behaviour - Disoriented
*Alertness- Decreased
*Speech and language - No response
2. Cranial nerve examination -
*Olfactory - Not elicited
*Optic
nerve Visual acuity, colour vision- Not elicited
Pupils- Bilateral pupils reacting to light
*Oculomotor,Trochlear,Abducens
No Nystagmus
*Trigeminal nerve
Sensory and Motor -Not elicited
Corneal and Conjunctival reflex- Present
*Facial nerve
No deviation of mouth
*Vestibulocochlear nerve
Rinne's and weber's test is not elicited
*Glossopharyngeal nerve
Gag reflex- Not elicited
*Vagus nerve
Not associated with dysphagia
*Accessory nerve
Trapezius - Not elicited
Sternocleidomastoid- Not elicited
*Hypoglossal nerve
No deviation of tongue
3.Motor examination
*Bulk - Normal
*Tone
Right Left
1. Upper limb Hypotonia Hypotonia
2. Lower limb Hypotonia Hypotonia
*Power
Right Left
1. Upper limb 2/5 2/5
2. Lower limb 2/5 2/5
*Reflexes
Superficial Right Left
1. Corneal +2 +2
2. Conjunctival +2 +2
Deep
1. Biceps. +2. +1
2. Triceps. +1. -
3. Supinator . +1. -
4. Knee. + +2
5. Ankle - Plantar reflexes - B/L withdrawal
4. Sensory examination
Not elicited
5. Cerebellum
Tremors- Absent
Knee jerk- Not elicited
Gait- Cannot be elicited
6. Meningeal signs Unable to look for meningeal signs as patient is uncooperative
Investigations:
3/9/21
Haemogram :
RBS :
LFT :
PC INR :
APTT - 30 sec
PT - 17 sec
INR - 1.22 sec
Blood grouping :B positive
Rapid dengue : NS1 +
Serum electrolytes :
Blood urea :
Serum creatinine :
Complete urine examination :
MRI Brain Plain :
Chest X-ray :
2 D Echo :
- No RWMA
- Trivial TR+ , No MR/AR
- Sclerotic AV , No AS/MS
- Good IV Systolic function
- EF 60%
- RVSP 35 mmHg
- No diastolic dysfunction
- No PAH/PE
- IVC size : 1.25 cm
TREATMENT :
- IVF NS,RL,ONS @ 150ml/hr
- INJ MANNITOL 100ml/IO/TID
- INJ PANTOP 40mg IU/OD
- INJ CEFTRIAXONE 2gm IV/BD
- INJ DEXAMETHAZONE 4mg IV/TID
- INJ ACYCLOVIR 400 mg IV/QID
- RT FEED 100ml water hourly, 50 ml milk 2nd hourly
- GRBS 6th hourly
- Strict I/O CHARTING
- BP/PR/TEMP hourly
- SYP LACTULOSE 100ml/RT/ H/S to maintain 2 stools /day
- INJ Vitamin k 10 mg/IV/OD
- INJ LEVIPIL 500mg IV/BD
- NEB Doulin 8th hrly
Budecort 12th hrly
Mucomyst 8th hrly
- Chest physiotherapy
- Air water bed
- Frequent position change 2nd hourly.
3/9/21
2 pm
- IVF 75 ml/hr
- INJ PAN 40mg OD
- FOLEY'S CATHETERIZATION
- RYLE'S CATHETERIZATION
- T PCM/RT/SOS
- GRBS 6th hourly
3/9/21
5 pm
- Pt drowsy
- GCS- F4V1M4
- CVS - S1,S2 (+)
- R/S NVBS (+)
- P/A soft
CNS - Tone increased in all limbs
Reflexes :
B T S A K P
R - 3+ 3+ 3+ - - Extension
L - 3+ 3+ 3+ - - Extension
Treatment :
- IVF NS, RL, DNS 150ml/hr
- INJ MANITOL 100ml IV/TID
- INJ DEXA 8 mg IV BD
- INJ CEFTRIAXONE 2gm IV/BD
- INJ ACYCLOVIR 400 mg IV/QID
- INJ PANTOP 40mg IV/OD
- BP/PR/TEMP/RR 4th hourly
- GRBS 6th hourly
- I/O CHARTING
Provisional diagnosis:
Altered sensorium under evaluation
?Encephalitis
?Metastasis of cancer cervix
4/9/21
9 am
- Pt is drowsy but arousable with painful stimuli( STU POUR ) , Afebrile
- PR - 79/min
- BP - 180/90 mm Hg
- CVS S1,S2 (+)
- R.S BAE (+) NUBS
- P/A - Soft,NT BS(+)
CNS
Doll's eye (+)
Corneal (+)
Conjunctival (+)
Gag Plantar(B/L)
Pupillary : NS, sluggish to light
5/9/2021
8 am
O/E : E2 V1 M4
Vitals :
- Temperature : 98.6°F
- BP : 140/80 mmHg
- PR : 74 Bpm ( Regular ) @ Volume
CVS : S1S2 heard , no Murmur
RS : NVBS (+) decreased Breathsounds in (lt) Esa ; B/L Grunting (+)
- P/A : soft , no Tend Bowel sounds (+)
GRBS : 169 mg/dl
I/O : 2250/1650 ml
CNS :
Dolls eye - present
Cornea - present
Conjuctival - present
Pupils - sluggish
REFLEXES :
B T S A P Le
Rt 3+ 3+ 3+ - Increased 2+
Lt 3+ 3+ 3+ - Increased 2+
TONE :
Rt Lt
UL. Hyper Hyper
LL Hyper Hyper
- Didn't pass stools
6/9/21
8 am
- Fever spike last night febrile to touch
- Spo2 98% with 2 litres O2
- O/E : E2 V1 M4
- BP : 140/60 mmHg
- PR : 88 Bpm
- CVS : S1 S2 +
- RS : NVRS+
B/L Grunting
- P/A soft , non tender
- Dolls eye - present
Cornea - present
Conjuctival - present
Pupils - sluggish
REFLEXES :
B T S K A P
Rt 3+ 3+ 3+ 2+ - Increased
Lt 3+ 3+ 3+ 2+ - Increased
TONE :
Rt Lt
UL. Increased Increased
LL. Increased Increased
7/9/21
8 am
GCB - 3/15
SPO2 - < 90%
Tachypnoea present
Respiratory distress present
Patient was intubated and put on mechanical ventilator
2:30 pm
Post intubatory vitals
BP - 130/80 mmHg
PR - 114bpm
CVS - S1, S2 +
RS - BAE +
6:05 pm
Absent central pulse
CPR was initiated
6:20 pm
CPR was continued
PR was NR
BP was NR
Inj. IV Epinephrine was given
6:25 pm
CPR was continued
PR was NR
BP was NR
Inj. IV Epinephrine was given
6:30 pm
CPR was continued
PR was NR
BP was NR
Inj. IV Epinephrine was given
6:35 pm
CPR was continued
PR was NR
BP was NR
Inj. IV Epinephrine was given
6:40 pm
CPR was continued
PR was NR
BP was NR
Inj. IV Epinephrine was given
6:46 pm
Despite all the above resuscitation, the patient could not be survived and was declared dead at 6:46 pm
Cause of death
Immediate cause of death - Cardiac arrest
Antecedental cause of death -
1. Encephalitis secondary to dengue
2. Multiple infarcts in Rt. Thalamus, B/L cerebellum
3. H/O CA cervix
4. Viral hepatitis
5. Grade 1 bed sore
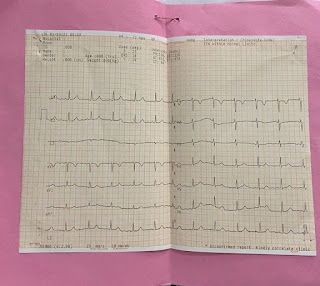
ECG at the time of death:
















Comments
Post a Comment